New Zealand needs about 1500 more hospital specialists, 1400 GPs and 12,000 nurses to match Australia per capita, the Association of Salaried Medical Specialists (ASMS) estimates.
The Government needs to declare a health workforce emergency as Omicron threatens to rip through the community, a senior doctors' union is urging. "These are serious numbers ... doctors tell us they have never seen it so bad ... there is a lot of anxiety about the weeks ahead," ASMS executive director Sarah Dalton told.
A Ministry of Health spokesperson said preparations were underway to manage the impact of Omicron to our health system, however, they declined to outline specifically how capacity would be strengthened. More detail would be announced on Wednesday, they said.
They also failed to respond to questions about how DHBs could create extra resources and whether they would consider declaring a health workforce emergency.
An outbreak of the highly infectious new variant of Covid-19 meant New Zealanders would face more cancelled and delayed surgeries, resulting in an even bigger backlog, she said.
"We need to declare a health workforce emergency along the lines of a civil defence emergency, to trigger official action on staff retention and recruitment and ensure it is prioritised at central Government and regional hospital and community levels," Dalton said.
It comes after Prime Minister Jacinda Ardern moved the country into the red traffic light setting on Sunday at 11.59pm as nine Covid cases in Motueka were confirmed to have the Omicron variant. Top health experts predict daily case numbers could reach over a thousand in about two weeks.
Director-general of health Dr Ashley Bloomfield on Sunday morning assured New Zealanders there was plenty of capacity in the health system to deal with the initial stage of the Omicron outbreak.
"ICU capacity was under 70 per cent at the moment," Bloomfield said.
Yet, Dalton painted a different, more "chilling", picture, saying the lack of adequate staffing meant extremely limited or no ICU (intensive care unit) capacity in some regions.
Emergency departments (ED) regularly operated at well over 120 per cent capacity and being desperately overstretched was the norm, not the exception, she said.
"The situation was magnified over the holiday period with departments trying to manage exceedingly high patient volumes with even more barren rosters," Dalton said.
Patients in some EDs were left waiting up to eight hours just to be seen and others spent hours in ambulance bays waiting to be triaged, she said.
"Then there are those who didn't wait and left hospital without their health needs being met – many of whom were mental health patients.
"We are told seeing people sitting in ED corridors clutching their chest and looking unwell while waiting to be assessed is a common occurrence," Dalton said.
Looking across the Tasman last week was chilling, she said.
In Victoria, there were more than 4000 healthcare workers who couldn't work due to Covid isolation requirements, with 5000 estimated absences every day on average, Dalton said.
"Health authorities took an unprecedented step of calling a system-wide 'Code Brown' to manage a system buckling under severe staffing shortages and hospitalisation rates amid the Omicron outbreak," she said.
Back in New Zealand, some regions were already struggling more severely than others.
In one region with very high needs, one child psychiatrist is trying to cover the work of three, Dalton said.
In Southland, maternity services were so precarious the hospital's unit almost had to be downgraded because a senior doctor was unable to get back into the country.
In Canterbury, ongoing staffing pressures saw cancer patients waiting up to 12 weeks just to get a first specialist appointment, while 365 patients were waiting for radiation therapy, with treatment delays of up to four months.
"Running a large waiting list is a direct consequence of an understaffed service operating above clinical capacity," Dalton said.
Cancer Society of New Zealand chief executive Lucy Elwood said cancer services in many areas were stretched because there wasn't enough senior medical doctors and it meant wait times continued to get worse.
"We're aware many radiologists work significantly more clinical hours than their overseas counterparts as a result of the workforce gaps," she said.
Eldwood said the society supported ASMS's calls for declaring a health workforce emergency.
"It's particularly significant at the moment, as in the near future it's easy to imagine a material number of senior medical officers needed to isolate due to Covid," Elwood said.
A Ministry of Health spokeswoman said they had been asking the New Zealand public to prepare for Omicron by continuing to wear a mask, scan and pass, and to get a booster shot if eligible and a test if any symptoms occurred.
"Having a highly vaccinated population is less likely to put severe strain on our health system and is just one part of overall planning for Omicron."
The spokeswoman said the ministry was also strengthening health system capability and capacity.
"Our health system is preparing for hospitalisations due to Omicron as well as the extra support that will be needed in primary care and emergency services.
"As it does now, the health system will continue to prioritise services based on capacity and clinical need. Planning is underway at local, regional and national levels," she said.
Health Minister Andrew Little told the Herald he had no power to declare a state of emergency and was not aware of the data the ASMS was referring to.
"I have been kept advised of hospital occupancy rates throughout the Christmas/New Year period and they have averaged around 80 per cent with a couple of hospitals experiencing 50 per cent occupancy over a number of nights.
"However, we know there is a work force shortage right across the health system following a decade of neglect and underinvestment from the previous Government.
Little said a strong focus had been put on preparing the country's health system to deal with Covid.
"Because of this preparation and the amazing work of our health workers our hospitals have not become overwhelmed due to the pandemic response," he said.
Little said the Government had provided surge training to roughly an additional 1400 nurses to work in an ICU /HDU environment to support ICU nurses if required.
"Given the experience of Omicron overseas is that it is less severe than the Delta variant, with a lower hospitalisation rate and an even lower ICU admission rate, I am confident from our experience to date along with the other measures in place to slow the spread of omicron our system will again respond appropriately."
=============================================
www.nzherald.co.nz...
=============================================
Riddle Alert! Who’s Up for Some Brain-Busting Fun?
4-letter word, always done tomorrow,
We’re out of tea, the ultimate sorrow!
Without the eye, you owe me some money,
No sugar no nectar no sweetness no honey,
4-letter word, if by chance you choose,
You can never win, you can only lose!
What is the 4-letter word?
Do you think you know the answer to our daily riddle? Don't spoil it for your neighbours! Simply 'Like' this post and we'll post the answer in the comments below at 2pm.
Want to stop seeing riddles in your newsfeed?
Head here and hover on the Following button on the top right of the page (and it will show Unfollow) and then click it. If it is giving you the option to Follow, then you've successfully unfollowed the Riddles page.

Poll: Should all neighbours have to contribute to improvements?
An Auckland court has ruled a woman doesn’t have to contribute towards the cost of fixing a driveway she shares with 10 neighbours.
When thinking about fences, driveways or tree felling, for example, do you think all neighbours should have to pay if the improvements directly benefit them?

-
82.4% Yes
-
14.9% No
-
2.7% Other - I'll share below
Live Q&A: Garden maintenance with Crewcut
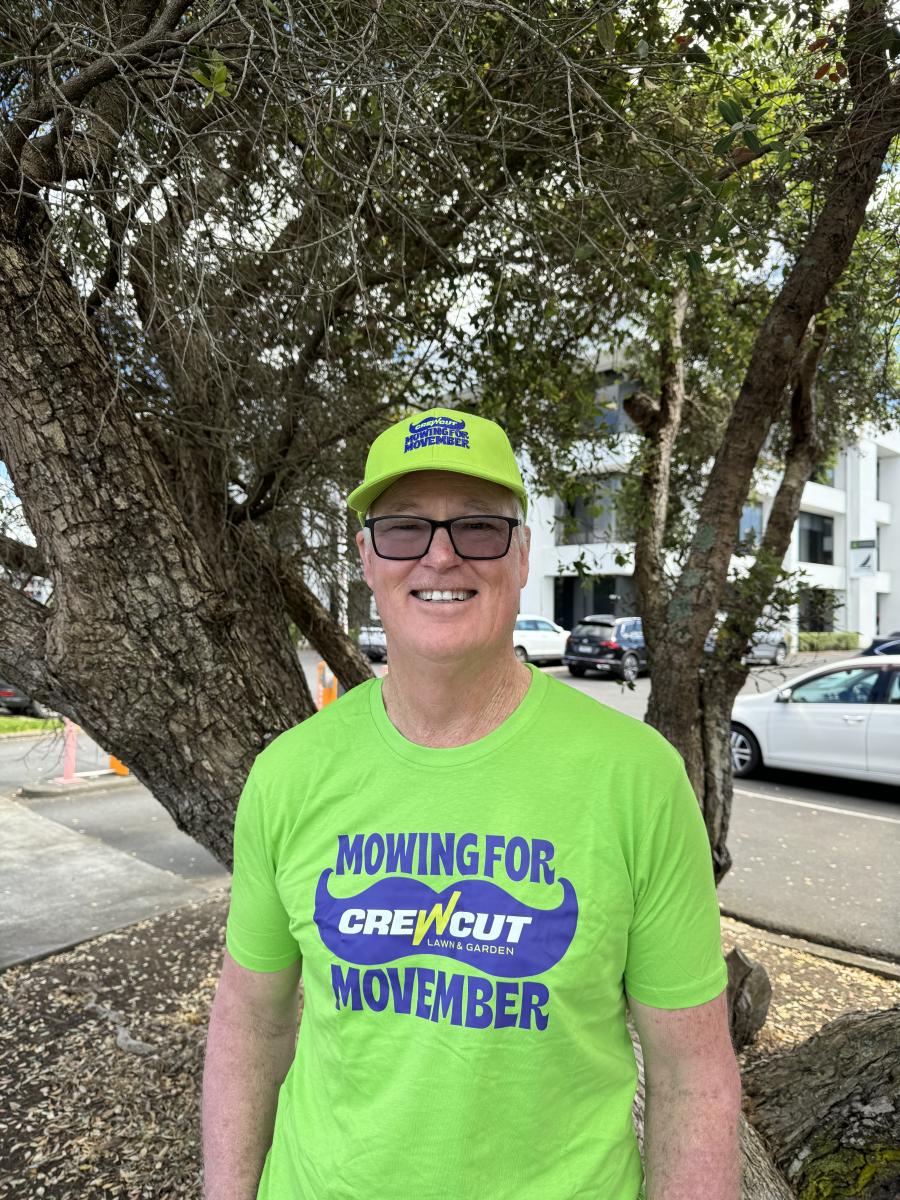
This Wednesday, we're having another Neighbourly Q&A session. This time with John Bracewell from Crewcut.
John Bracewell, former Black Caps coach turned Franchisee Development Manager and currently the face of Crewcut’s #Movember campaign, knows a thing or two about keeping the grass looking sharp—whether it’s on a cricket pitch or in your backyard!
As a seasoned Crewcut franchisee, John is excited to answer your lawn and gardening questions. After years of perfecting the greens on the field, he's ready to share tips on how to knock your garden out of the park. Let's just say he’s as passionate about lush lawns as he is about a good game of cricket!
John is happy to answer questions about lawn mowing, tree/hedge trimming, tidying your garden, ride on mowing, you name it! He'll be online on Wednesday, 27th of November to answer them all.
Share your question below now ⬇️






 Loading…
Loading…


















